
The Difference Between Optimal and Struggling EHR Instances
For many in healthcare, there remains a belief that nobody has a successful EHR experience. As we’ve discussed previously, highly satisfied organizations do exist! We have gathered more and more Arch Collaborative data and in the process, we’ve learned that providers can have a positive EHR experience on nearly any vendor’s offering.
This begs the question, “What are the successful organizations doing differently?”
We’ve discussed the three big areas that lead to improvement:
- Training
- Personalization
- Governance
But I thought it would be helpful to discuss some of the anecdotal data we’ve gathered as we’ve worked with both high- and low-satisfaction organizations. How do these types of organizations behave differently? Well, for one, the end users of the five highest satisfaction and five lowest satisfaction Arch Collaborative member organizations have drastically different views on the EHR:
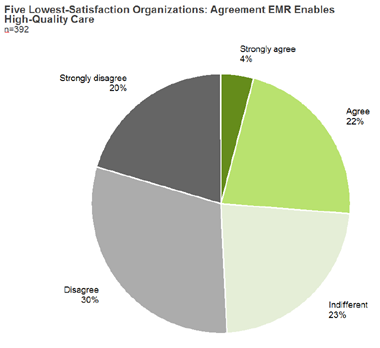
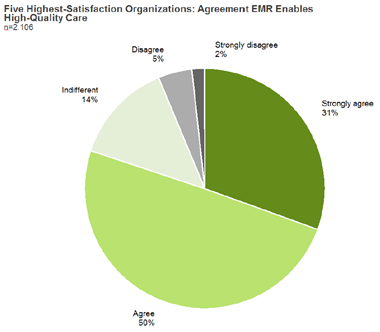
We can safely say that the five lowest-ranking organizations aren’t full to the brim with luddites, just as we know that not everyone in the five highest-ranking organizations are tech-utopia idealists. No, these dramatic shifts in opinion about the EHR stem from broader, harder-to-quantify issues – like misaligned organization culture.
We’ve found that high-performing organizations report:
- Optimism that they can make their users successful – even seeking out the least successful clinicians;
- A constant focus on building trust with clinical users;
- A strong focus on helping users figure out how to effectively learn and use the EHR;
- Surprise when they’re informed their clinicians report above-average satisfaction. “There is so much more we could and should be doing!”
Case in point: I recently spoke with a CMIO from a high-performing organization, and our meeting had run a bit long. I knew he was supposed to be other places, but he absolutely could not get off the phone without sharing his vision for the organization’s next step in bolstering EHR usability across their health system.
By contrast, we’ve found that low-performing organizations report:
- A strong focus on new technologies that can solve EHR satisfaction;
- A feeling of acceptance that clinicians will never be happy with the EHR;
- A focus on vendor failings.
These negative sentiments are reflected by low-satisfaction clinicians. For example, here are a few things we’ve heard from those we’ve surveyed:
“The EMR will be the downfall of patient care.”
“If there has ever been a profession at the mercy of IT designers, it is medicine.”
“Until I can really use this tool and set it up for my workflow, using it will be like running in someone else’s shoes that are tied together.”
I think that last remark in particular hits the nail on the head. The implementation of an EHR represents the complete upheaval of the clinician workflow. The need for an organization to integrate their system in a way that supplements clinician workflow can’t be overstated.
Let’s take that quoted provider’s metaphor about shoes a step further. Outdoor enthusiasts have widely varying needs, from the thick-soled waterproof hiking boot to the form-fitting, grippy climbing shoes of a rock climber. Still, each group needs shoes. In much the same way, the workflow of a cardiologist and a primary care physician vary widely, but they both need to chart.
EHR vendors are in the position of trying to sell a core system that needs to do everything for everyone; a hiking, jogging, climbing hybrid, so to speak. What we’re often left with is a shoe that leaves everyone with blisters. Leaders in a health system should take a good look at their “do-everything” tool and decide for each workflow the fat that needs trimming.
The responsibility for EHR success rests on many shoulders; vendors, provider leadership, clinicians, and governments. However, at the end of the day, KLAS has seen that the organizations who don’t wait for other stakeholders to lift their load often have enough they can do to positively impact the outcomes of their end users.