Why Can't Note Bloat Be Tamed?
Does the following comment on desired EMR improvements sound familiar?
“I review charts for a living and the copy and paste function is far misused and abused. It can be very difficult to find what is going on currently with the patient, when significant events occurred and what the physician’s plans are to act on the changes in the patient's condition. The daily note has become bloated and useless.”
Cut and paste functions were designed to improve charting efficiency, but quickly became a misunderstood and often misused function of the EMR. Determining why organizations have not invested in building note templates that are efficient and placed emphasis on how and when to use copy and paste charting function is an enigma in most provider organizations.
Why do physicians do it?
- CYA - They are protecting themselves and the organization from medical liability, "the bigger the note the more I am covered.” However, the risk if an encounter goes to court is that the documenting of redundant previously recorded peer notes obfuscates the medical findings and can result in the physician and the organizations losing the case.
- More Money - They may feel that the more your document, the higher the reimbursement.
- Ease - The speed of copy and paste, while enticing on the input side, creates issues on the output side.
- "Not My Notes" - The author of the note is not the end user of the note, so there is little incentive to change practice. Yet at the same time each physician complains of their peer’s notes being useless.
- Not asked to fix it - They have not been engaged to create a clinically relevant note that meets the needs for coding, billing and research.
- Lack of Training - They have not been trained on how to use the templates and tools available to them.
A potential path for taming note bloat:
- Bring in the users of the note output to provide a perspective on what is needed in a note
- First - What are the “musts” for
- Clinical communication
- Coding and billing
- Legal requirements
- Second – Design and build standard templates
- Third – Train the physicians on how to use the templates
- Forth – Educate on the appropriate used of copy and paste
- Finally – Audit and provide feedback to physicians for improvement, directly and with department chairs
- First - What are the “musts” for
Another area of focus that can help includes engaging with the research staff to determine where they see problems with note bloat in the chart. Are note bloat problems related with specific diagnoses, departments, areas, physicians? If so, can treatment protocols and/or clinical protocols supported by EMR personalization tools be used to manage or eliminate note bloat?
Copy and paste misuse and note bloat continues to cause frustration for many clinicians and organizations. It will take a team of stakeholders to create a solution for improvement of clinical communication while meeting the needs of coding, billing, compliance and research. Organizations need to adequately support the efforts to improve clinical documentation tools, templates and education to reduce note bloat.
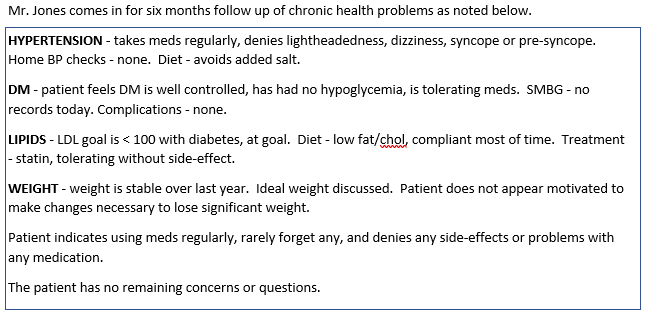
An example of concise assessment and planning by one family practice specialist is shown below. The note is a standard HPI template used by the physician. Modifications are made to the sections of the template as needed during the examination to make the note unique to the encounter. This physician routinely sees more patients than his partners every month.
EMR Ambulatory Macro HPI Charting Template Example: