 2024 BEST IN KLAS
2024 BEST IN KLAS
Preferences
Related Series


Breast Tomosynthesis 2013
The Business Case
Breast tomosynthesis has created a lot of energy within the women’s imaging community. While the clinical benefits are becoming more apparent, the reimbursements are inconsistent, and it is expensive to adopt this technology. Providers want to know: Is it worth the investment? Is a positive ROI possible? Hologic is currently the only vendor with FDA approval for tomosynthesis; therefore, KLAS interviewed 50 Hologic tomosynthesis customers from 44 unique organizations about their experience.
Key Findings
The Benefits Outweigh the Concerns—About 85% of providers said they were able to achieve a positive ROI. Early adopters had concerns about the extra time tomosynthesis can take as well additional costs and the necessity for more storage. Several providers reported finding cancers they would not have seen with traditional 2D digital mammography, stating the clinical benefits help offset concerns. All but one said they would buy tomosynthesis again.
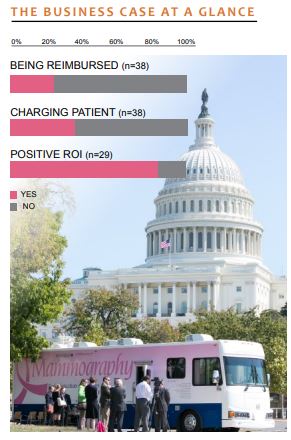
Reimbursements Are Still Inconsistent—Despite the mounting evidence that tomosynthesis is better for patients, reimbursements are unpredictable. After two years of tomosynthesis in clinical use, providers are still waiting to see progress. Only 25% said they are reimbursed for tomosynthesis above the standard mammo reimbursement but that they could not count on that consistently.
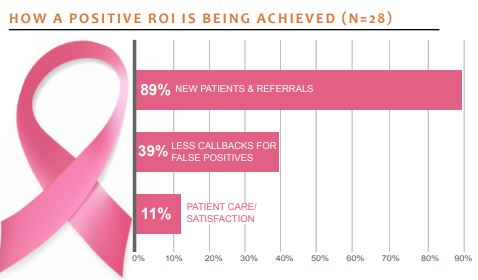
Finding ROI in Tomosynthesis—ROI is not a result of traditional reimbursement or charging patients, and organizations that charge patients do not necessarily see a greater ROI than those that do not. Tomosynthesis has indirectly helped the bottom line because providers are able to attract new patients and are making fewer false-positive callbacks.
Payment Realities
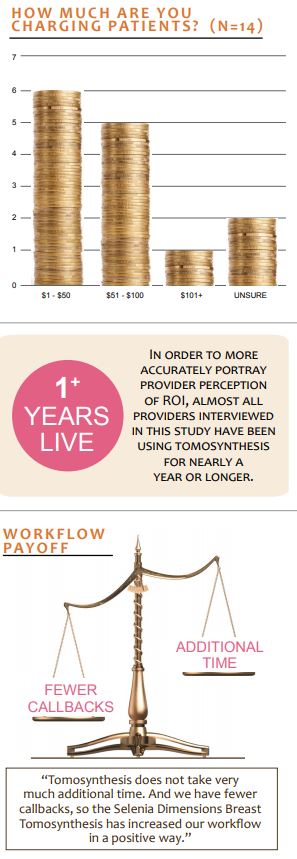
About 37% of providers in this study said they were directly charging patients for tomosynthesis. The vast majority of those said they charge less than $100. Getting paid by private insurance or CMS is difficult because there is no standard for billing tomosynthesis.
A couple of providers described a workaround using a miscellaneous code in order to bill insurance; however, there is still no rhyme or reason to when or why they are reimbursed. Out of the ten who were reimbursed, one indicated it was from CMS. Those reimbursed were from Ohio, Colorado, Iowa, Illinois, Texas, and West Virginia. However, providers from the same states reported differing experiences with reimbursements.
How Providers Are Achieving a Positive ROI
Even though most providers are not charging patients extra, and are not consistently being reimbursed, nearly 90% of those surveyed said they are achieving a positive ROI. Providers saw a significant reduction in false-positive callbacks, an increase in new patients, and even workflow improvements. These three elements work hand in hand to help providers achieve a positive return.
Fewer False-Positive Callbacks—Thirty-nine percent of providers who say they are getting a positive ROI said that fewer callbacks are part of the reason why. A few providers reported that callback rates have dropped about 25%– 40%. While false-positive callbacks do still happen, they occur less often. One provider said, “We have about 30% fewer callbacks. We have been tracking this closely. Our physicians who did not buy in before have bought in now because of the fewer callbacks, and because of [cancers] they have found that they feel may have been missed without tomosynthesis.”
More New Patients—Eighty-nine percent of providers who said they are getting a positive ROI say that the tomosynthesis technology has garnered new patients and referrals. Adding tomosynthesis creates a buzz that is good for recruiting new patients. One provider said, “First, our recall rate has significantly decreased, so instead of seeing patients again for false positives, we are able to get new patients in. Also, we are the first in the area to have tomosynthesis, and we have seen an influx of new patients since we implemented it. These factors combined have allowed us to see a [revenue] increase of 7% when most imaging departments are seeing a decline.”
Better Workflow—More than 50% of providers reported that the workflow was positively impacted by tomosynthesis. After getting over the learning curve, the acquisition time was reported to be only a slight increase over traditional mammography scans. For radiologists, the reading takes significant extra time in the beginning but that extra time decreases as they acclimate to the technology. Many said that the reduction in callbacks and the detection of cancers that would have been missed had they used 2D imaging make up for any marginal increase to the scan time. One provider said, “Our workflow has been much better because the reduced number of callbacks has saved us a tremendous amount of time. The extra time to perform the scan is not a factor since it adds only seconds to our workflow.”
The Bottom Line
Providers are seeing cancers they would not previously have seen with traditional digital mammography. Also, though there are extra costs and challenges that go along with tomosynthesis, providers see a positive return financially as well as clinically. Overall, based on the experience from their peers, providers who are considering tomosynthesis would benefit by quickly jumping on the bandwagon. There is some question about what will happen to ROI when the market is saturated, as well as why reimbursements are not happening on a consistent basis, but tomosynthesis is on its way to being the new standard of care for breast imaging.
This material is copyrighted. Any organization gaining unauthorized access to this report will be liable to compensate KLAS for the full retail price. Please see the KLAS DATA USE POLICY for information regarding use of this report. © 2024 KLAS Research, LLC. All Rights Reserved. NOTE: Performance scores may change significantly when including newly interviewed provider organizations, especially when added to a smaller sample size like in emerging markets with a small number of live clients. The findings presented are not meant to be conclusive data for an entire client base.




